With the integration of high-level diagnostic technology and therapeutic interventions for dry eye disease (DED), the optometrist must be aware of the related coding best practices and clinical documentation for both. This will ensure reimbursement for their services.
Coding Best Practices
Careful International Classification of Diseases (ICD)-10 selection supports the optometrist’s Current Procedural Terminology (CPT) usage and reduces claim denials. The optometrist should use the most specific code that describes the DED subtype and etiology and avoid unspecified codes when possible.
Here are common ICD-10 codes for DED:
• H04.121–H04.129 – Keratoconjunctivitis sicca due to aqueous tear deficiency
• H16.221–H16.229 – Keratoconjunctivitis sicca, not due to Sjögren’s syndrome
• M35.01 – Sjögren’s syndrome (systemic link)
• Z79.899 – Long-term medication use (eg, antihistamines, isotretinoin)
• L29.0 – Pruritus associated with lid margin disease
Additionally, the optometrist should link procedures, such as punctal plugs or matrix metalloproteinase-9 testing, with appropriate diagnosis codes (eg, H04.123 for moderate aqueous-deficient DED). Also, every technology and treatment should be linked to a diagnosis and change in management plan.
Further, the optometrist must include interpretation and management decisions in their clinical notes and add photographs and printouts from imaging devices to the patient’s chart. By remaining consistent and specific, the optometrist has a strong defense against an audit.
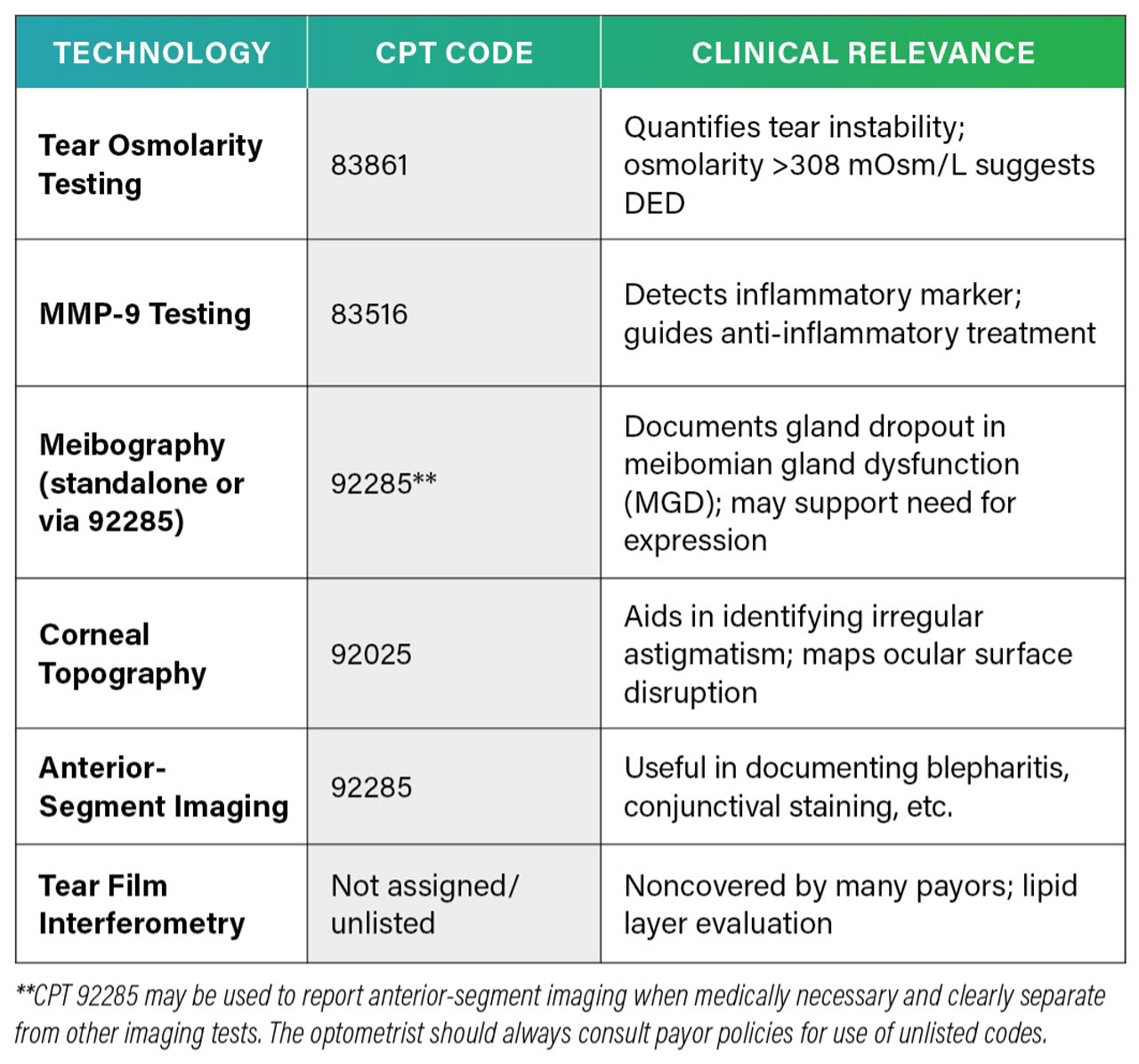
Clinical Documentation for Diagnostics
Present-day DED coding for reimbursement requires the optometrist to identify the root cause of the condition and use the correct CPT code (see Table 1 below).
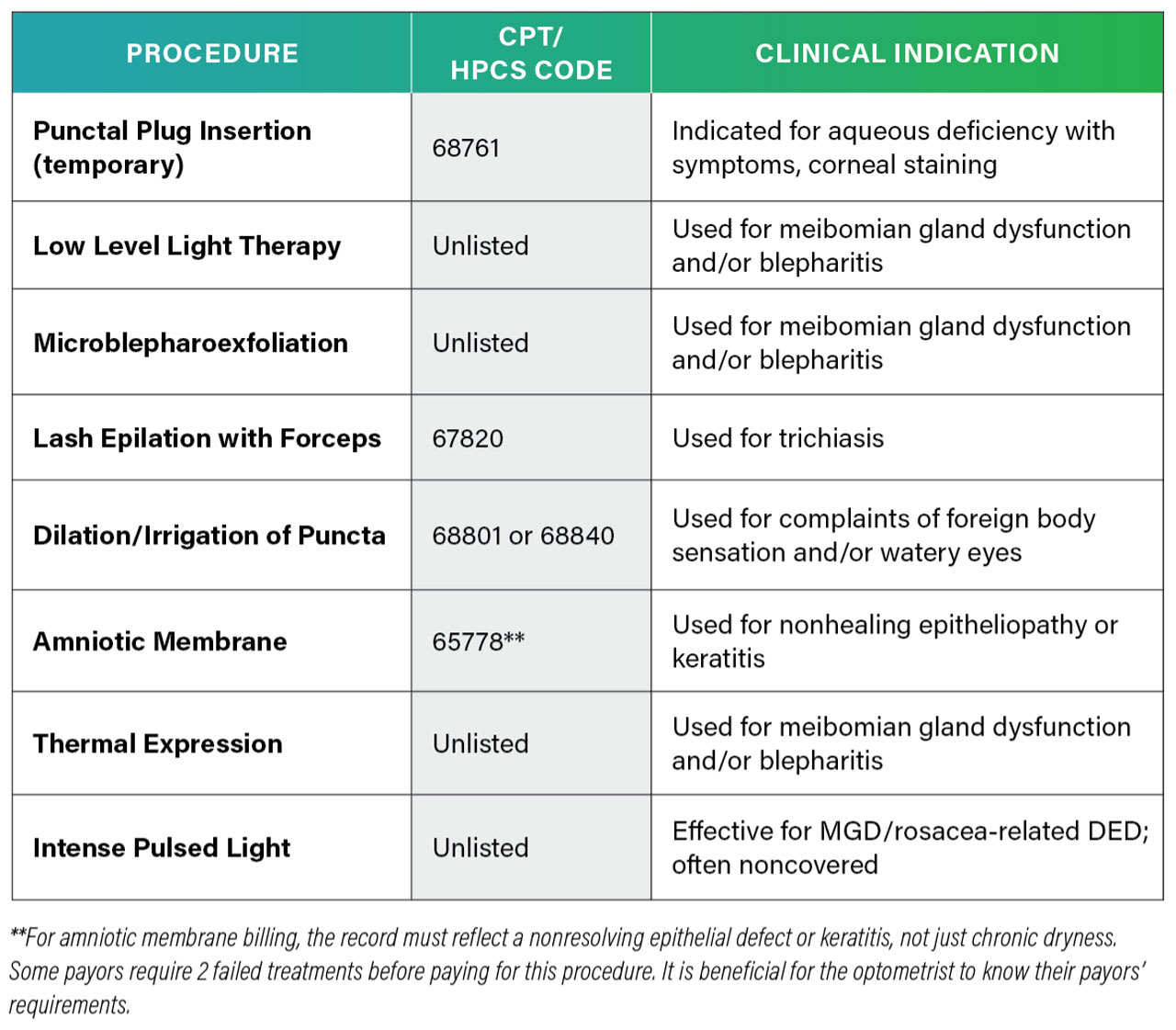
Clinical Documentation for Therapeutics
With DED therapy, coding must reflect not just the service provided, but also the severity of disease and failure of prior conservative therapy. (See the descriptions of procedures, CPT/HCPS codes, and clinical indications listed in Table 2, below.)
A Medically Necessary Condition
The clinical and financial management of DED demands that the optometrist balance technology integration with reimbursement strategy. Reimbursement depends on strong documentation, proper code selection, and understanding the limitations of each payor’s policy. By framing dry eye disease as a medically necessary condition—supported by data, diagnostics, and outcomes—the OD can lead in both patient care and practice growth. OM